Holmium laser enucleation of the prostate (HoLEP)
What is involved in the HoLeP procedure?
Your prostate gland surrounds your urethra as it exits the bladder. When it enlarges (BPH), it can obstruct the urine flow. HoLEP entails threading a telescope through the urethra and utilising a laser to gently extract the central portion of the prostate gland, effectively forming a broadened channel for improved urine flow. Typically, a temporary bladder catheter is inserted at the conclusion of the operation.
HoLEP is typically reserved for larger glands where TURP can not be performed safely. A/Prof Homi Zargar, does not performs this procedure and offers an alternative procedure called robotic simple prostatectomy for larger prostate gland at Epworth,Richmond hospital.
After treatment urinary flow improves by 90%
Robotic simple prostatectomy is an alternative to HoLEP
HoLEP main points
Key Points:
HoLEP includes the removal of obstructive prostate tissue using a laser fiber passed through a telescope inserted via the penis.
HoLEP proves highly effective in enhancing urinary symptoms associated with bladder outflow obstruction, particularly for men experiencing urine retention and relying on a urinary catheter.
Following the procedure, a bladder catheter will be in place for 24 to 72 hours to flush out any blood clots.
Common post-operative effects include a loss of emission during ejaculation and short-term experiences of bleeding, burning sensations, or increased urinary frequency.
A/Prof H.Zargar can assess whether the size and shape of your prostate make you a suitable candidate for this procedure. Depending on the size of the prosatate gland, alternative procedures can be performed.
surgery
What occurs on the day of the procedure?
Details of the procedure:
A general anaesthetic (keeping the patient asleep) or a spinal anaesthetic (rendering the patient unable to feel anything from the waist down) is typically administered.
An injection of antibiotics is usually administered before the procedure, following a thorough check for any allergies.
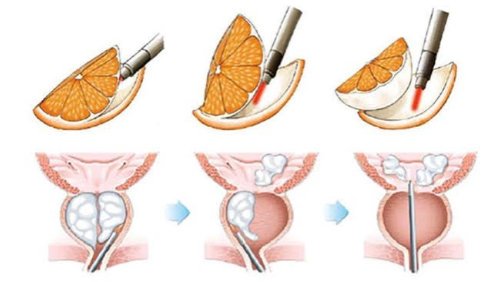
A telescope is passed into the bladder through the urethra , and a laser fiber is used to peel away pieces of obstructing prostate tissue (prostate lobes) from the surrounding prostate capsule; the peeled pieces are flushed into the bladder.
The morcellation (chopping up) and suctioning out of prostate pieces occur using a specialized instrument (a morcellator) introduced into the bladder through the telescope.
The removed prostate tissue undergoes microscopic pathology analysis.
After the prostate is removed, any bleeding points in the surgical cavity are carefully treated with the laser.
A catheter is inserted into the bladder at the end of the procedure.
Bladder irrigation through the catheter is typically performed for a brief period after surgery to flush through any clots or bleeding.
On average, the procedure takes about two hours to complete, depending on the size of the prostate.
Hospitalization usually extends to one night, but in some cases, the surgery can be performed as a day case.
The bladder catheter is typically removed within the first 1-2 days after surgery. Initial pain and increased frequency while passing urine are common, and relief can be achieved with painkillers such as Paracetamol; frequent urination usually begins to improve within a few days.
The laser technique removes a significant amount of tissue, impacting urinary control initially. Improvement occurs as pelvic floor muscles recover, settling for most men over a short period.
Bloody urine for 24 to 48 hours post-catheter removal is common, and some patients may experience difficulty passing urine at this stage. If this occurs, a temporary catheter is inserted to allow swelling related to the operation to settle. Typically, patients go home with this catheter and return a week or so later for a successful second catheter removal; this approach proves effective in almost all cases.
After-Effects and Risks of the Procedure:
Temporary mild burning, bleeding, and frequent urination
Occurs in almost all patients
No semen production due to retrograde ejaculation (passes back into the bladder on ejaculation)
Risk: In 9 out of 10 patients (90%)
Continuing blood in your urine for several days after surgery
Risk: Between 1 in 2 & 1 in 10 patients
Temporary short-term loss of urinary control, which can be improved with pelvic floor exercises
Risk: Between 1 in 10 & 1 in 50 patients
Treatment may not relieve all symptoms
Risk: Between 1 in 50 & 1 in 250 patients
Bleeding requiring a blood transfusion or re-operation
Risk: Between 1 in 50 & 1 in 250 patients
Anaesthetic or cardiovascular problems possibly requiring intensive care (including chest infection, pulmonary embolus, stroke, deep vein thrombosis, heart attack, and death)
Risk: Between 1 in 50 & 1 in 250 patients (individual risk estimation by your anaesthetist)